My School Nurse Told Me I Was “Faking It”… Then My Heart Stopped In The Hallway
“That’s not what I meant. Obviously, in retrospect, he did have a medical condition. But at the time, based on the information I had, my assessment was reasonable. I can’t be expected to diagnose rare genetic conditions in a school nurse’s office. That’s not my job.” She stammered.
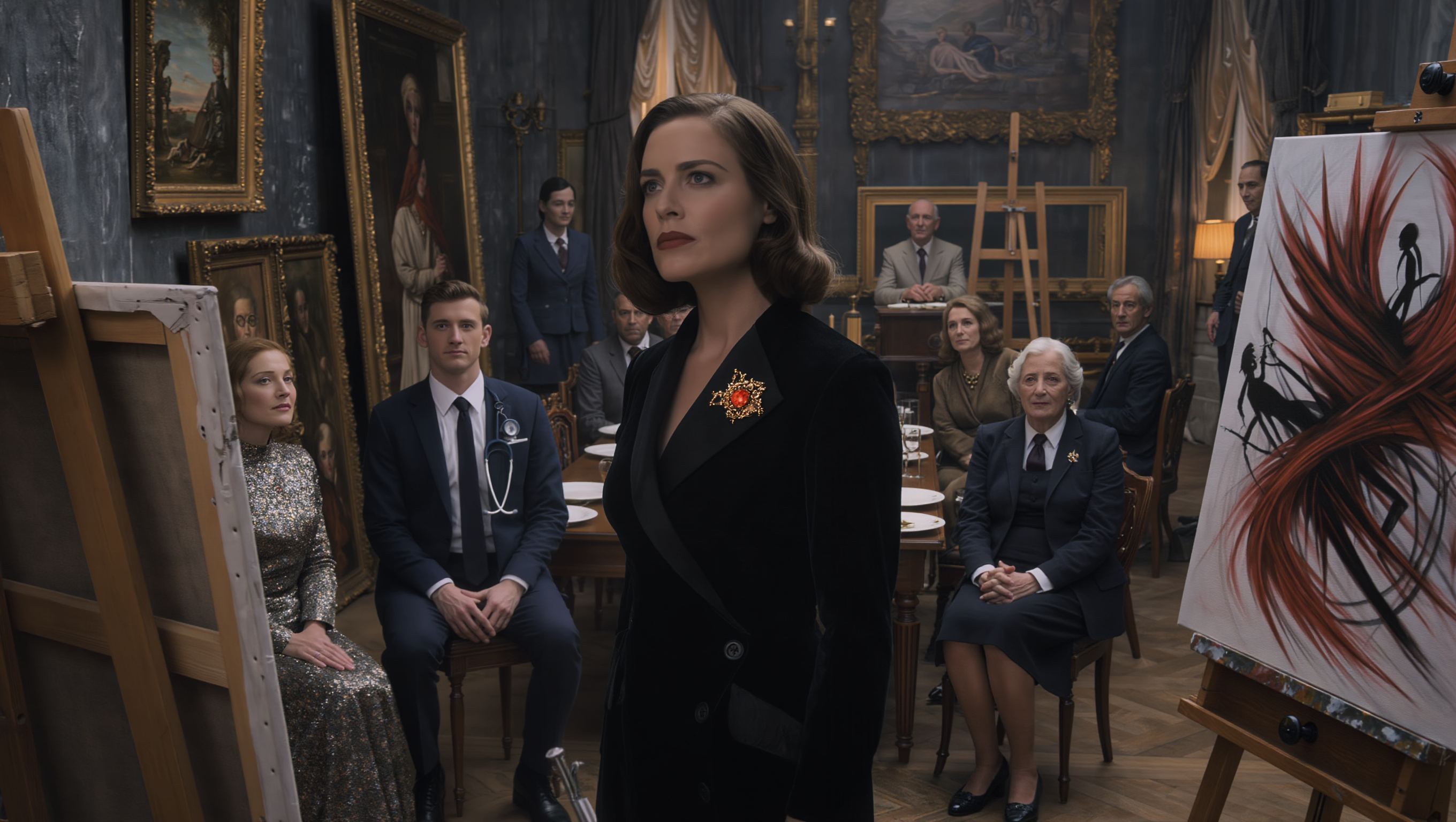
Francis’s voice was cold.
“Your job is to provide competent medical care to students. A student presented with cardiac symptoms. You failed to perform even basic cardiac assessment. Because of your failure, he went into cardiac arrest 20 minutes later. His heart stopped. He died on your hallway floor. How is that reasonable?” She stated.
The recording went on for another hour, Campbell getting more defensive and contradicting herself repeatedly. She admitted she’d been concerned enough to Google smartwatch accuracy after I left, but not concerned enough to call me back.
She acknowledged that chest pain combined with irregular heartbeat would typically warrant cardiac assessment, but insisted my specific presentation hadn’t seemed serious. She claimed teenagers were prone to exaggerating symptoms, but then said I hadn’t seemed distressed enough to be genuinely ill.
She tied herself in logical knots trying to justify her decisions, and with every answer, she made Francis’s case stronger. By the end, even her own lawyer seemed to have given up trying to rehabilitate her testimony.
The damage was done. She’d admitted to making assumptions based on my age rather than my symptoms, to failing to perform basic medical assessments, to prioritizing her own convenience over patient care.
Her 18 years of experience had become 18 years of developing bad habits that had nearly killed me. The school district’s defense was somehow worse.
Their lawyer argued governmental immunity, claiming the district couldn’t be held liable for the actions of individual employees. Francis demolished that argument by showing the district had received three formal complaints about Nurse Campbell in the previous five years, all regarding dismissive treatment of students with legitimate medical conditions.
The district had done nothing except require Campbell to attend a single continuing education seminar on adolescent health. They’d been aware of a pattern of poor care and had failed to take meaningful action.
The district’s risk manager testified that they’d considered replacing Campbell but decided against it because she was close to retirement and finding qualified school nurses was difficult in the current market. They’d prioritized administrative convenience over student safety.
The risk manager actually said on record that they’d calculated it would be cheaper to handle occasional lawsuits than to hire a new nurse. That statement became Exhibit A in the punitive damages phase.
Meanwhile, my junior year of high school had started without me. I’d been cleared by Dr. Patel to return to school in September, but my parents insisted on keeping me home for the first few weeks while the media attention was still intense.
By the time I finally went back, the viral video had mostly faded from public consciousness, though kids at school definitely still remembered. Walking through the hallways, I felt everyone’s eyes on me.
Some kids stared at the visible bump of my ICD under my shirt; others whispered to their friends when I passed. A few came up to tell me they were glad I was okay, or to share their own stories of being dismissed by Nurse Campbell.
The school had hired a new nurse, a young guy named Nurse Gregory, who’d apparently been briefed extensively on my case because he introduced himself during my first day back. He assured me his office door was always open if I ever had any concerns whatsoever about my health.
He seemed nervous, like he was terrified I’d collapse on his watch too. Classes were harder than they used to be.
I’d missed enough school that I was playing catch-up in every subject, but beyond that, I just couldn’t focus the way I used to. My mind kept drifting to my heartbeat, hyper-aware of every skip and flutter.
The beta blockers made me tired all the time. I’d fall asleep in afternoon classes, my body heavy and slow.
I couldn’t do gym class anymore. The doctor’s note excused me from any physical activity more strenuous than walking.
I’d been on the cross-country team before, running varsity since freshman year, but that was over now. No contact sports, no competitive running, nothing that would elevate my heart rate too much.
Sitting in study hall while my former teammates practiced outside the window, I felt like I’d lost part of my identity. Being a runner had been who I was.
Now I was the kid with the heart condition, the kid who’d gone viral dying on camera, the kid everyone had to be careful around because I might drop dead at any moment. The lawsuit dragged on through fall.
Francis filed for summary judgment, arguing the facts were so clearly in our favor that a trial wasn’t even necessary. The judge denied the motion, saying a jury should decide questions of negligence and damages.
Jury selection was scheduled for January. Meanwhile, Nurse Campbell’s nursing license hearing was happening separately.
The state nursing board had opened an investigation after my cardiac arrest made news. Her license was suspended pending the outcome of the hearing.
Francis encouraged my parents to provide testimony at the hearing. My mom testified about finding out her son had died in the school hallway, about the genetic condition that had killed her brother now manifesting in her child.
My dad testified about Campbell’s complete failure to provide appropriate care. Then they played the hospital security footage.
The footage showed me arriving via ambulance, still in V-fib, the paramedics shocking me in the ER. It showed Dr. Okonquo working on me, calling for Dr. Patel, ordering tests.
It showed the moment I regained consciousness, disoriented and scared. The nursing board watched the entire video in silence.
Then they watched the cell phone footage from school, the viral video, seeing me collapse and seize and receive CPR. Campbell sat at the defendant’s table, forced to watch the consequences of her negligence play out on screen.
“Miss Campbell, after watching this footage, do you believe you provided appropriate medical care to this patient?” One of the board members asked her directly.
She consulted with her lawyer before answering.
“I believe I made a reasonable clinical decision based on the information available at the time.” She said.
The board member’s expression hardened.
“The appropriate answer was no.” He said.
The board deliberated for three hours before issuing their decision: license revoked, effective immediately. Campbell could petition for reinstatement in five years, but she’d have to complete additional education and demonstrate she’d remediated the deficiencies that led to her negligent care.
The board chair read a statement explaining their reasoning.